Understanding Third-Party Administrators and Modern Healthcare Insurance Solutions
Healthcare insurance has evolved dramatically over the past decade, transforming from simple coverage plans into comprehensive ecosystems that prioritize patient care, transparency, and accessibility. As medical costs continue to rise globally, the role of third-party administrators has become increasingly vital in bridging the gap between insurance providers, healthcare facilities, and policyholders. These specialized organizations handle the complex administrative tasks associated with health insurance, ensuring that claims are processed efficiently, networks are managed effectively, and members receive the support they need when it matters most.
Comprehensive Coverage Through Life Line Insurance Services
When considering healthcare protection for yourself and your family, life line insurance represents a critical safety net that provides peace of mind during medical emergencies and routine healthcare needs. Modern insurance administration has transformed dramatically, moving away from complex paperwork and lengthy approval processes toward streamlined digital solutions that prioritize member experience. The contemporary approach to healthcare coverage emphasizes transparency, accessibility, and efficiency, ensuring that policyholders can access quality medical care without unnecessary bureaucratic obstacles.
A robust insurance administration system processes thousands of claims daily using sophisticated adjudication rules and automated systems that reduce manual intervention while maintaining accuracy. This technological advancement means that members experience faster claim approvals, reduced waiting times, and fewer administrative headaches when seeking medical care. The emphasis on automation does not diminish the human element rather it allows customer service teams to focus on complex cases that require personal attention and expertise.
The Role of Khat Al Haya in Healthcare Management
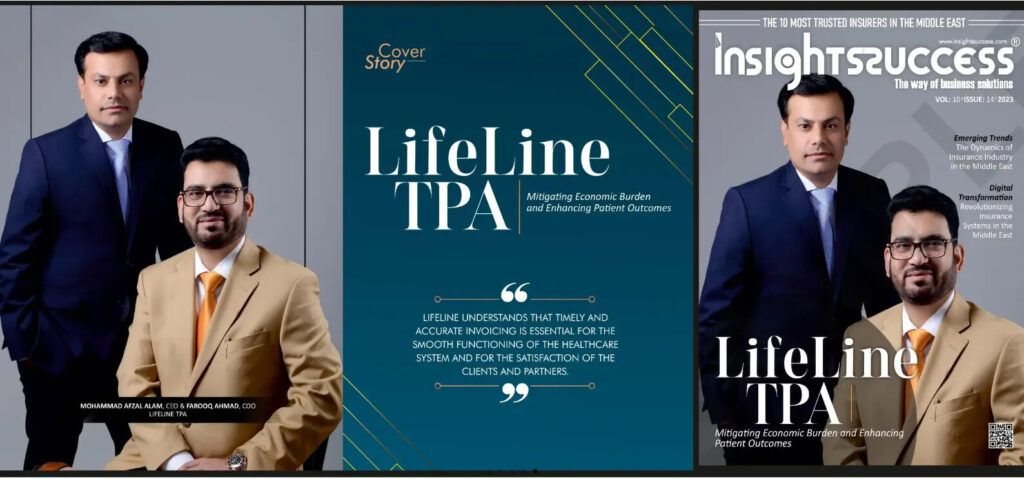
Operating across multiple countries in the Middle East region, khat al haya represents a commitment to excellence in healthcare insurance administration that has been refined over years of dedicated service. Established with the vision of transforming how health insurance claims are managed, this specialized third-party administrator has built its reputation on reliability, efficiency, and member-centric service delivery. The organization’s presence in the UAE, Oman, and Turkey demonstrates its capability to navigate different healthcare systems while maintaining consistent service quality.
The foundation of successful healthcare administration lies in understanding the unique needs of diverse populations and adapting services accordingly. Whether serving individual policyholders, families seeking comprehensive coverage, or large corporate groups requiring customized benefit packages, the ability to tailor solutions while maintaining operational efficiency sets exceptional administrators apart from average providers. This flexibility extends to claims processing, where intelligent systems handle routine approvals automatically while experienced medical professionals review complex cases that require clinical judgment.
Accessing Healthcare Through the Lifeline Network List
The accessibility and quality of healthcare services depend significantly on the breadth and depth of provider networks available to insured members. The lifeline network list encompasses a comprehensive array of healthcare facilities including hospitals, clinics, pharmacies, and specialized medical centers across the GCC region. This extensive network ensures that members can access cashless medical services at participating facilities, eliminating the financial burden of upfront payments and subsequent reimbursement claims. The convenience of cashless transactions cannot be overstated, as it removes a significant barrier to seeking timely medical care.
Network management extends beyond simply listing healthcare providers to include ongoing quality assessments, contract negotiations, and service level monitoring that protect member interests. Regular evaluations ensure that participating facilities maintain appropriate standards of care, that pricing remains competitive and fair, and that members receive consistent service quality regardless of which network facility they choose. This active management approach creates accountability within the network and drives continuous improvement in healthcare delivery.
The integration of technology into network management has revolutionized how members interact with healthcare providers. Online portals and mobile applications allow policyholders to search for nearby network facilities, check coverage details, verify eligibility before appointments, and even schedule consultations directly through digital platforms. This technological enablement puts control in the hands of members, allowing them to make informed choices about where and when to seek medical care based on their specific needs and preferences.
Round-the-Clock Support and Advanced Claims Processing
Exceptional customer service distinguishes premium healthcare administrators from basic service providers. A dedicated customer care center operating twenty-four hours a day, seven days a week, three hundred sixty-five days a year ensures that members can access support whenever they need assistance. Whether dealing with a medical emergency in the middle of the night or seeking clarification about coverage details during business hours, immediate access to knowledgeable support staff provides reassurance and practical help when it matters most.
The claims processing infrastructure represents the technological heart of modern healthcare administration. Advanced systems equipped with thousands of adjudication rules automatically process the majority of claims without manual intervention, dramatically reducing processing times and minimizing errors. This automation capability handles routine claims efficiently while flagging unusual cases for human review, ensuring both speed and accuracy in claims settlement. The result is faster reimbursements, fewer disputes, and higher member satisfaction.
Transparency in communication stands as a fundamental principle that guides all interactions between administrators, members, and healthcare providers. Clear explanations of coverage terms, honest discussions about limitations and exclusions, and open communication about claim statuses build trust and prevent misunderstandings. When members understand what their coverage includes, how to use their benefits effectively, and where to seek help with questions or concerns, they can navigate the healthcare system confidently and make the most of their insurance investment.
Continuous staff training and development ensure that customer service representatives, claims processors, and medical review teams maintain current knowledge about healthcare trends, insurance regulations, and best practices in service delivery. This commitment to professional growth translates directly into better service for members, as knowledgeable staff can resolve issues quickly, answer questions accurately, and provide guidance that helps policyholders maximize their healthcare benefits.
The future of healthcare administration lies in the seamless integration of technology, expertise, and human compassion. As medical treatments become more advanced and healthcare costs continue rising, the role of efficient administrators becomes increasingly important in ensuring that quality medical care remains accessible and affordable for individuals and families across the region.
